Reimagining the Future of AI-enabled Medicine
Physicians, researchers, academics, and industry leaders gathered to discuss the future of artificial intelligence in health care.
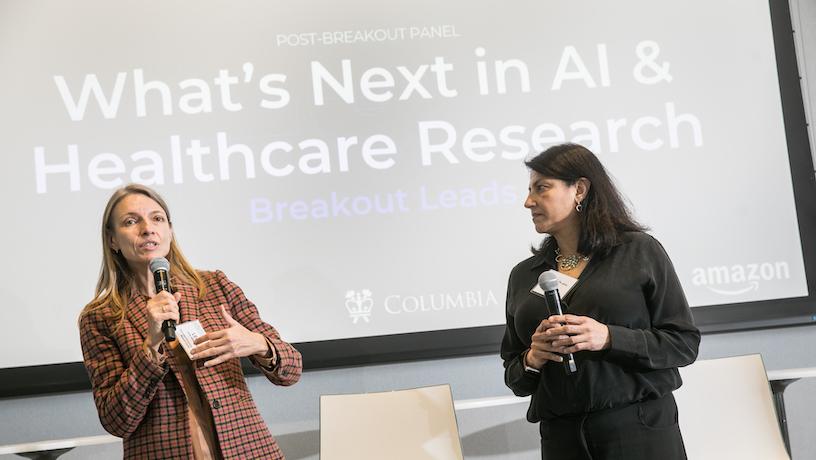
Lena Mamykina (CUIMC) and Sunita Mishra (Amazon Health Services), moderators of breakout session "How might we create interactive intelligent systems for re-imagined patient-clinician encounters?" Credit: Timothy Lee
How will AI change health care?
That was the driving question at the third annual Columbia Center for Artificial Intelligence Technology (CAIT) research symposium, held Oct. 26 in Geffen Hall on Columbia’s Manhattanville campus. In a day of keynotes, panel discussions, and breakout sessions, attendees discussed topics ranging from electronic medical records and patient empowerment to emergency room staffing algorithms and patient trust in AI-enabled healthcare.
The event was an opportunity for experts from Amazon, Columbia Engineering, Columbia University Irving Medical Center, and Columbia Business School to discuss the most promising applications and vexing challenges that are emerging as AI stands poised to become a central part of the health care experience for patients and providers.
“CAIT has three main goals,” said Shih-Fu Chang, dean of Columbia Engineering and center director. “Those are advancing the state-of-the-art, developing the next generation of leaders, and propagating knowledge about AI to broader fields.”
“Today, we’re taking a deep dive into health care and particularly the opportunities and challenges presented by medical information,” Chang said.
The flow of information
Attendees at the poster session. Credit: Timothy Lee
Electronic medical records are one of the most promising applications of AI and a rich source of training data for research and development.
“In the immediate term, the AI application I’m most excited about in primary care is the ability to easily sort through the immensity that exists today in medical records,” said Andrew Diamond, chief medical officer at One Medical, which Amazon acquired earlier this year. “It’s much easier for a primary care doctor to make a medical decision when they have easy to digest data in front of them.”
Sunita Mishra, chief medical officer at Amazon Health Services, said her team is working to relieve the administrative burden by using AI tools to “automate all the pieces that can be automated – including chart-hunting and following up on telephone notes.”
“When making a decision about whether to refill a medication or to order a lab, the provider has information at their fingertips, rather than having to go hunting through the chart,” she said.
That’s vital because medical notes that were once one or two sentences have ballooned to documents that run hundreds of pages. Using AI to summarize these notes into concise summaries of care “is going to be, in the short term, the most transformative thing AI can do,” Diamond said.
Building patient trust

Sunita Mishra (Chief Medical Officer, Amazon Health Services), Katrina Armstrong (Dean, Vagelos College of Physicians and Surgeons, CUIMC), Andrew Diamond (Chief Medical Officer, One Medical), and moderator Shih-Fu Chang (Dean, Columbia Engineering). Credit: Timothy Lee
Another key theme of the day was the challenge of building trust with patients who might already be wary of the medical system or who don’t like the idea of AI systems supporting their medical care.
Mishra pointed out that patients might have different expectations when it comes to interacting directly with automated systems to receive health care.
“It may be just fine if you’re going in for acne treatment. If you’re getting a low-acuity service, many people may be very comfortable getting it treated through technology,” she said. “In other instances, they want more of a high-touch experience.”
Of course, the status quo doesn’t necessarily provide that. Katrina Armstrong, dean of the Vagelos College of Physicians and Surgeons and executive vice president for health and biomedical sciences at Columbia University Irving Medical Center, says she recently noticed while working in a hospital that a lack of communication across large care teams is already undermining patient trust.
“Dr. A shows up at 9 o’clock and says you don’t need this test and Dr. B shows up at 10 o’clock and says you do need it,” said Armstrong.
“We need tools that bring the team together and share the data so that when Dr. B is talking to a patient, they can talk through the reasons Dr. A may think something different. It’s not to hide anything but rather to help the patient understand why the reasons might differ.”
Armstrong emphasized that it’s vital to give patients reason to believe these new tools are at least as capable as human clinicians and that they are aligned with patient interest.
“If we let these tools become perceived as a way to ration care, or to do things based upon profit, we’re going to really further erode trust in the medical system,” she said.
“We’ve got to figure out the values, not just the competence.”